Do check the Apollo Munich health insurance claim application form for treatment expenses already paid by the policyholder, Download the form and apply for reimbursement…
Apollo Munich Health Insurance is a well-preferred now called HDFC ERGO and taken insurance policy by many individuals, who are employed or hold any business, and there are numerous hospitals that fall under the Apollo Munich network area and do provide cashless transactions for the entire treatment.
There are two main Apollo Munich Health Insurance claims that are provided which are cashless claims for the treatment that is pre-planned and other is during the emergency, and thus patients can anytime visit the network hospital and get their treatment done with a cashless transaction and if the hospital does not accept the cashless transaction, they can pay their treatment bills and get them reimbursed.
Apollo Munich Health Insurance Claim Procedure
There are two types of claims that are being considered by the health insurance company, once they provide an Apollo Munich Health Insurance Policy, where to raise a claim, it is necessary to be aware of the transaction type and the procedure you have gone through during your treatment.
Cashless Treatment
The cashless transaction is for the network hospital that accepts your policy number and allows you to get the treatment done without paying any bills, and in this treatment, the patient need not pay any amount during their treatment except for some exceptional medicine or test bills, and for any queries, you may contact health insurance customer care at any time.
These bills can also be reimbursed later as per your current policy taken, and if your treatment does fall under the Apollo Munich Health Insurance Policy, the entire expenditure will be considered and there is no need to pay anything by hand.
Claim for Treatment Expenses
There are cases that even the network hospital of Apollo Munich Health Insurance does reject the cashless transaction due they’re not proper policy details. If the treatment is done in an emergency, the hospital does advise to pay the bills by cash and then use the Apollo Munich Health Insurance claim form to reimburse the same.
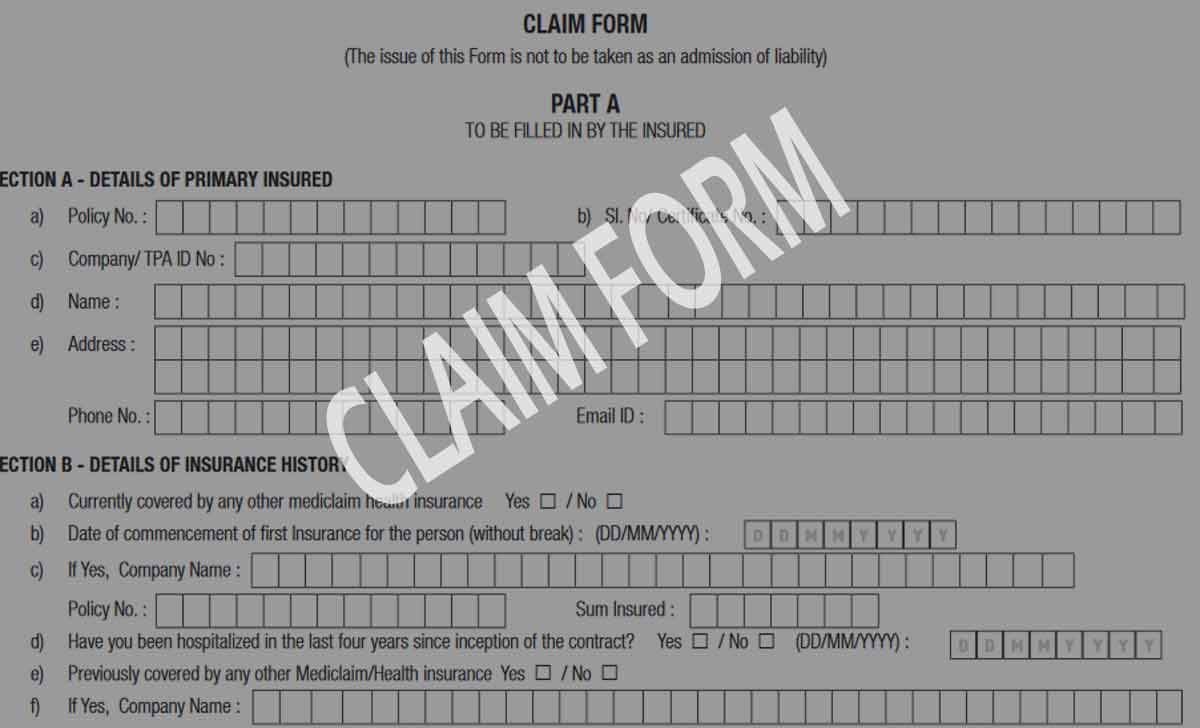
Find Apollo Munich Health Insurance Claim Application Form at https://fhpl.net/Forms/AMHI_OC(platinum)claimform.pdf
Below is the detailed procedure that will be followed for the treatment done through cash for Apollo Munich Health Insurance policyholders.
Policyholders or their guardians must reach to the Apollo Munich Health Insurance toll free number to register their emergency claim and thus intimate them that you have been through this treatment, such that an emergency claim case does get raised.
Use the Apollo Munich Health Insurance email address with your date of admission to get the case registered.
Upload your entire treatment bills and summary of the hospital to the insurance policyholder, such that they examine and verify your entire details, and the Apollo Munich Health Insurance will verify the documents submitted through verification and reach the hospital where you have taken the treatment.
Fill the Apollo Munich Health Insurance Claim Form and submit it along with the documents thus to mention your policy number for better reach and easy reimbursement, and once the claim has been confirmed, the insurance provider will initiate the reimbursement amount as per the agreed values.
Documents Required
There are a few must attach documents that must be added along with the Apollo Munich Health Insurance Claim form, and here is the list of the documents provided which must be with you, while asking for the reimbursement: Claim form online
- Apollo Munich Health Insurance Claim Form with Policy Number
- Claim Form duly signed by insurance provider and insured
- Hospital Bills and discharge summary of entire treatment
- Medicine and Test Bills that took during the treatment
- Bank account stamen or cancel check for reimbursement
Do we need to get a hospital stamp on claim Form?
Yes, the Apollo Munich Health Insurance Claim form does have a section or hospital where their entire details must be mentioned, and as well the attestation of the hospital needs to be made, as proof of treatment is taken by the insured as per the hospital and expenses bills.
How Many days does an Apollo Munich Health Insurance claim take?
A total of 30 to 45 days is the minimum number of days considered for the entire Apollo Munich Health Insurance reimbursement process to work, and as the documents verification online and offline along with proper policy details form insured to match with treatment has taken will get you the amount fixed which might be less in many cases with respect to the amount spent during treatment.
Can we reclaim the submitted claim in Apollo Munich Health Insurance?
Yes, the claim that is sent to reimbursement under Apollo Munich Health Insurance policy of the insured can be taken backward until the payment process has been initiated, and if the policy holder isn’t satisfied with the amount considered for reimbursement by the insurance provider, then they can ask to stop the claim process and they reinstate it with proper justification.